Diversity, Equity and Inclusion
Every patient deserves to be seen.
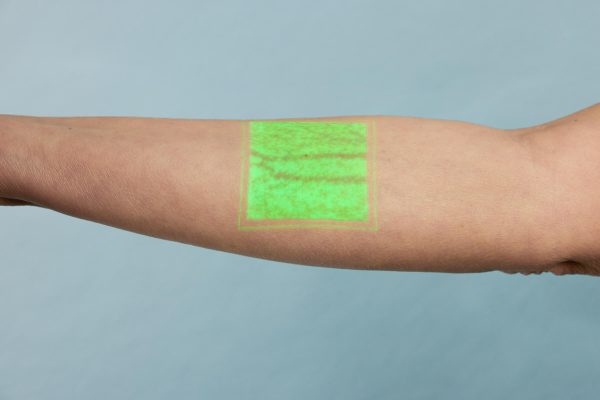
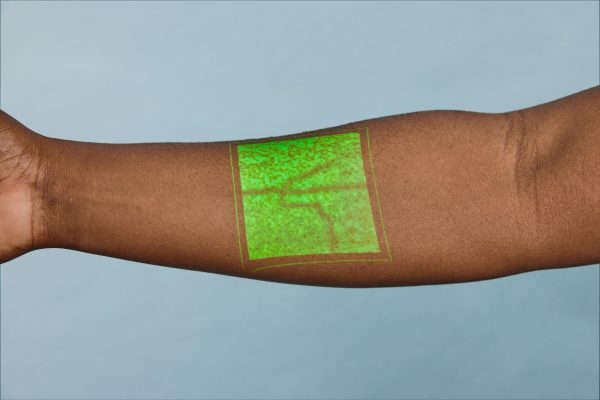
Up to 50% of first IV catheter stick attempts fail,1 and first attempt failure rate is up to 21% higher in patients with dark skin pigmentation2
- Multiple insertion attempts can lead to treatment delays, increased risk of infection, and patient and staff dissatisfaction.1,3
- First attempt failure complications are associated with patient demographics including skin color, age, and BMI.4
- CDC data shows that 49.9% of non-Hispanic Black adults suffer from obesity,5 a condition that makes obtaining vascular access especially challenging.
AccuVein is equally beneficial to patients of all skin pigmentation


“Every patient deserves the right to safe, equitable health care. All health care organizations have a responsibility to identify and address the disparities that their unique patient populations face.”
DR. JONATHAN B. PERLIN, MD, PhD
President and CEO – The Joint Commission
©The Joint Commission, 2023. Reprinted with permission.

Support Healthcare Equity




PIVC placement is the most commonly-perfomed invasive procedure in medicine1 with up to 90% of patients receiving IV therapy during their hospital stay.6,7
Failed sticks result in a cascade of clinical and operational issues8-11,13-15
Increased pain and stress
for patients and staff8

54% increase in complications
when 2 or more puncture attempts are performed14

Increased escalation calls
to other staff or central resources10
One in two catheters fail
to make it to 5 days or to the end of treatment7-9
Almost one quarter
of hospital acquired BSIs were in patients with PIVCs11
Up to 43% of PICCS are “non-essential”
and placed due to difficult or failed PIVC access in some care settings12,13
2. Kaddoum, R.N., Anghelescu, D. L., Parish, M. E., Wright, B. B., Trujillo, L., Wu, J., … & Burgoyne, L. L. (2012). A randomized controlled trial comparing the AccuVein AV300 device to standard insertion technique for intravenous cannulation of anesthetized children. Pediatric Anesthesia, 22(9), 884-889.
3. Haskins, R.J. and Selby,L. (2021) Reducing peripheral venous catheter infections. Contagion 6(5), available from: https://www.contagionline.com/reducing-peripheral-venous-catheter-infections.
4. Eren, H. (2021). Difficult Intravenous Access and Its Management. In (Ed.), Ultimate Guide to Outpatient Care. IntechOpen. https://doi.org/10.5772/intechopen.96613
5. Stierman, B., Afful, J., Carroll, M. D., Chen, T. C., Davy, O., Fink, S., … & Akinbami, L. J. (2021). National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. Available at: https://stacks.cdc.gov/view/cdc/106273 (Accessed: November 8, 2022)
6. Marsh N, Webster J, Ullman AJ, et al. Peripheral intravenous catheter non-infectious complications in adults: A systematic review and meta-analysis. J Adv Nurs. 2020;76(12):3346-3362 doi:10.1111/jan.14565.
7. Alexandrou E, Ray-Barruel G, Carr PJ, et al. Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes Worldwide. J Hosp Med. 2018; 13(5): doi:10.12788/jhm.3039.
8. Cooke, M., Ullman, A. J., Ray-Barruel, G., Wallis, M., Corley, A., & Rickard, C. M. (2018). Not” just” an intravenous line: Consumer perspectives on peripheral intravenous cannulation (PIVC). An international cross-sectional survey of 25 countries. PloS one, 13(2), e0193436.
9. Sabri, A., Szalas, J., Holmes, K. S., Labib, L., & Mussivand, T. (2013). Failed attempts and improvement strategies in peripheral intravenous catheterization. Bio-medical materials and engineering, 23(1-2), 93-108.
10. Guillon, P., Makhloufi , M., Baillie, S., Roucoulet, C., Dolimier, E., & Masquelier, A. M. (2015). Prospective evaluation of venous access difficulty and a near‐infrared vein visualizer at four French haemophilia treatment centres. Haemophilia, 21(1), 21-26.
11. Stuart, R. L., Cameron, D. R., Scott, C., Kotsanas, D., Grayson, M. L., Korman, T. M., … & Johnson, P. D. (2013). Peripheral intravenous catheter‐associated Staphylococcus aureus bacteraemia: more than 5 years of prospective data from two tertiary health services. Medical Journal of Australia, 198(10), 551-553.
12. Reeves T, Morrison D, Altmiller G. A Nurse-Led Ultrasound-Enhanced Vascular Access Preservation Program. Am J Nurs. 2017 Dec;117(12):56-64. doi: 10.1097/01. NAJ.0000527490.24610.51. PMID: 29189249.
13. Govindan S, Snyder A, Flanders SA, Chopra V. Peripherally Inserted Central Catheters in the ICU: A Retrospective Study of Adult Medical Patients in 52 Hospitals. Crit Care Med. 2018 Dec;46(12):e1136-e1144. doi: 10.1097/CCM.0000000000003423. PMID: 30247241; PMCID: PMC6317857
14. Eisen LA, Narasimhan M, Berger JS, Mayo PH, Rosen MJ, Schneider RF. Mechanical complications of central venous catheters. J Intensive Care Med. 2006; 21(1):40–46. https://doi.org/10.1177/0885066605280884
15. Riley, L. and Schears, G.J. (2021) Failed peripheral intravenous catheter placement leads to inappropriate peripheral inserted central catheters use and patient harm: a retrospective database analysis [Poster presentation]. Association for Vascular Access 2021. https://ava2021-ava.ipostersessions.com/Default.aspx?s=E7-83-95-73-6C-6A-D7-24-9B-30-C2-E8-CB-82-26-41.
